The incidence of sexually transmitted infections is only increasing every year. A special place among these diseases is occupied by urogenital trichomoniasis, which is provoked by vaginal trichomonads. According to statistics, the infection is present in approximately 10% of the population, with an annual incidence of almost 200 million people. In Russia, for every 100 thousand people there are about 71 infected.
The disease is especially dangerous for women because it provokes serious complications, including vaginitis, urethritis and cervicitis. Also, many experts note that this infection can become one of the causes of inflammatory diseases of the pelvic organs, adverse outcomes of pregnancy, premature birth and cervical cancer. As for men, they are more often asymptomatic and do not provoke such severe complications.

What is trichomoniasis?
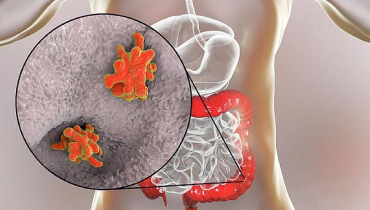
We have already noted that the disease is classified as an STI and is caused by a protozoan unicellular parasite – Trichomonas vaginalis. More than 50 varieties of trichomonads are known, but only 3 of them occur in humans: urogenital, oral and intestinal. T. vaginalis belongs to the first category and is a protozoan microorganism of three forms:
- ameboid
- pear-shaped
- budding
These pathogens form a cyst-like form, but are very sensitive to environmental conditions. However, they can parasitize on epithelial cells and replicate the topography of the host cell. This often makes it difficult to detect trichomonads during microscopy.
Once in the body, T. vaginalis infects exclusively the urogenital canal. The incubation period after infection may be quite short (1 to 3 days) or longer (4 to 28 days). However, the onset of the disease often goes undetected, which complicates treatment and often leads to serious complications.
The pathogenesis and symptoms of trichomoniasis are directly related to the virulence of the pathogen and the individual susceptibility of the body. For example, in women, the provoking factors for the development of infection may be hormonal disorders, vaginal pH violation in the alkaline side, avitaminosis and some associated pathologies of the genitourinary system.
Urogenital trichomonads have proteases (that is, enzymes that can break down peptide bonds), due to which they become tissue parasites. Trichomoniasis pathogens attach themselves to the surface of epithelial cells and overcome the body’s defenses through virulence. “Entrance gates” for T. vaginalis are the external genitalia, so the common way of infection is unprotected sexual contact with an infected person. However, infection of a child from infected parents or during childbirth is also possible.
In response to the introduction of urogenital trichomonads, there is a hyperreaction, but it is of a delayed type. Regardless of the causative agent, the reaction is limited to infiltrative inflammation. This results in hyperemia, edema, and an inflammatory infiltrate. Congestive hyperemia, which is provoked by the dilation of blood vessels and their overflow of blood, is not uncommon.
The disease has several clinical forms: there are acute, subacute and chronic stages. The acute form is characterized by the appearance of marked symptoms and rapid development. Without treatment, women may have chronic trichomoniasis, which is asymptomatic and has exacerbation stages.
It is worth noting that the severity of clinical manifestations depends on the form of the pathology: often the symptoms lose specificity due to the presence of mixed infection. According to statistics, “pure” trichomoniasis is observed in about 3-10% of cases. Most often, T. vaginalis interacts with other viruses or is a carrier of them, which leads to the emergence of several pathologies at once.
The most common female form of the disease is trichomonad colpitis. When it occurs, the patient may have profuse, liquid or foamy discharge, which has an unpleasant odor, and in rare cases – an admixture of blood. The presence of an inflammatory process is usually confirmed by examination of the external genitalia and mucous membranes.
In about 40-45% of cases, the development of vulvitis is observed. In the majority of cases, the inflammation becomes a consequence of the spread of the inflammatory reaction, as a result of which trichomoniasis proceeds in the form of vulvovaginitis. In this case, the patient complains of itching and burning at the vaginal opening. Unpleasant symptoms intensify during intimacy. In addition, pronounced external hyperemia is detected.
Another form of pathology is trichomonad vestibulitis. It occurs as a result of an isolated lesion of the microorganisms Vestibulitus vaginae. In this case, there is an increased sensitivity of the mucous membranes, often – bleeding.
If a woman does not have any inflammatory reactions in the body, we are talking about trichomonad carriage. Such a condition is considered a temporary carrier of the pathogen. In the future, it is possible to cure or manifest a clinical picture of the disease.
Unfortunately, trichomoniasis is a rather underestimated problem in the field of STD treatment. And very often it is given little attention in programs for the control and prevention of sexually transmitted infections. But every year the problem becomes more and more widespread. Many experts say that the infection significantly increases the risk of HIV infection, so it is worth paying more attention to the problem of its treatment and prevention.
Another peculiarity of trichomoniasis is that its successful treatment does not lead to the development of pronounced immunity. That is, secretory and serum antibodies are detected in sick or over-infected patients, but they are only evidence of a past or existing infection. However, these antibodies cannot provide lasting immunity, so there is a risk of reinfection.
Symptoms of the disease in women
In about 30-50% of cases, the infection is asymptomatic, which makes it difficult for early detection. In the presence of clinical manifestations, the following subjective symptoms are most often observed in female patients:
- Itching and burning in the genital area.
- Atypical vaginal discharge (most often have a grayish-yellow color, often frothy with an unpleasant odor).
- Unpleasant sensations during urination.
- Pain and burning when having intercourse.
- Pain, discomfort in the lower abdomen.
The intensity and severity of the symptoms depend directly on the menstrual cycle. Therefore, in the chronic course of the infection, recurrences occur exactly after the end of the menstrual cycle. This is explained by the fact that T. vaginalis is very dependent on organic iron, which they need to start developing. This component is found in excess in menstrual blood, which makes it a source of nutrition for pathogenic microflora.
There are also a number of objective signs of infection with trichomonads, that is, those that the doctor can detect in a woman during an examination. Among them:
- Hyperemia (redness) and swelling of the vulvar and vaginal mucosa.
- Foaming yellow-green discharge.
- Erosive and ulcerative lesions of the external genitalia.
- Petechial hemorrhages on the vaginal mucosa.
In parallel with such symptomatology, pelvic inflammatory pathologies, cystitis and pyelonephritis may be observed. Because of this, the clinical picture is often “blurred”, which does not allow making a differential diagnosis only on the basis of consultation and examination of the patient.
How can one become infected?
The main route of T. vaginalis infection is sexual, i.e. transmission occurs directly during sexual intercourse. In about 5% of cases there is intrapartum infection, in which the infection is transmitted to the baby from the infected mother during childbirth. In exceptional cases, there can be contact transmission (e.g. through towels or bed linen).
There are a number of factors that increase the risk of infection. These include:
- Promiscuous sexual relations, frequent change of partners.
- Sexual contact without a condom.
- The presence of inflammatory diseases of the urogenital system.
- Atrophy of the cervix.
- Immunodeficiency disorders (especially the presence of HIV).
There is also a proven link between the risk of infection and disorders of the acid-base balance in the vagina. Causes of such disorders may include endocrine system malfunctions, recent abortion, pregnancy or menstruation.
Diagnosis of the disease
Initial diagnosis of trichomoniasis occurs during a consultation with a gynecologist. The specialist clarifies the existing symptoms, collects the patient’s medical history, and then performs an examination on a gynecological chair. During the examination, objective symptoms of infection may be detected, but even in their absence, the doctor may suspect pathology and prescribe a number of additional diagnostic procedures.
Laboratory analysis for trichomonas plays a key role in the diagnosis of the disease, since many women are asymptomatic and the clinical picture is often nonspecific and similar to other STIs. That is why the diagnosis is made on the basis of the results of the examination, and not only on the basis of the examination and detected symptoms.
The clinical material for laboratory tests is a scrape (smear) from the urethra, cervical canal and vagina. One of the following tests is used to detect pathogens:
- Microscopic examination of a native preparation. This method has the highest sensitivity and specificity, but requires the examination of biological material immediately after it is obtained. Microscopic examination is used in the presence of a pronounced form of infection. The native preparation is prepared using isotonic sodium chloride solution or Ringer-Locke’s solution, which is mixed with biomaterial and applied to a slide. The resulting suspension is then covered with a coverslip and examined under a microscope. Often this examination is combined with the study of stained smears, which increases the likelihood of detecting trichomonads.
- Molecular biological methods. They are aimed at detecting specific fragments of DNA or RNA of pathogens in a smear. Special test systems are used for diagnosis. To this group of studies include the method of polymerase chain reaction (PCR), nucleic acid amplification (NASBA), as well as other similar techniques.
- Cultural examination. This method involves the use of nutrient media to culture trichomonads. Microscopic examination of the material is performed only 48 and 96 hours after seeding. It is used when the disease is asymptomatic or when the presumed diagnosis of trichomoniasis has not been subjected to microscopic examination. This technique is labor-intensive and time-consuming, so it is of limited use.
To improve diagnostic accuracy, a woman is advised not to use sprinkles on the eve of her visit to the doctor. As a rule, trichomonads in a smear are detected during the study of biomaterial from the mucosa of the posterior fornix of the vagina. However, in some cases, the separation obtained from the cervical canal is examined.
Also an important place in the diagnosis is taken by ultrasound of the pelvic organs. This technique is used to determine the condition of the bladder, fallopian tubes and endometrium. It is required in order to identify complications and concomitant pathologies that may affect the treatment process. In addition, a blood test may be required to determine the infectious status of the patient.
Differential diagnosis with other urogenital diseases is also important. It is primarily about infections provoked by pathogenic and opportunistic microorganisms, as well as viruses:
- Vaginal discharge changes can occur with gonorrhea, chlamydia, and fungal lesions, so they do not always indicate trichomoniasis.
- Itching and burning are also not specific symptoms of pathology, as they occur with HPV infection, fungal infections, or the presence of other diseases.
- Genital ulcers can be a consequence of herpes infection or syphilis, so differential diagnosis with these pathologies will be required.
If necessary, a consultation with other specialists may be prescribed:
- Obstetrician-gynecologist (in case of planning or pregnancy);
- A urologist (if inflammatory processes in the pelvic organs are suspected or the disease has a long course).

How is trichomoniasis treated?
The scheme of treatment of trichomoniasis in women is made individually, taking into account the existing symptoms, concomitant pathologies. The indication for therapy is the detection of T. vaginalis microorganisms in a smear taken for analysis.
The main objectives of therapy are the eradication (that is, the complete destruction) of pathogens, the prevention of the development of complications and the prevention of partner infection. When formulating the regimen, the doctor adheres to several principles:
- If trichomonads are detected in combination with Candida fungi, the patient is initially prescribed anti-candida therapy.
- A few days before the start of antitrichomonad therapy, a hepatoprotector is started. The selected drug will need to be taken during the entire treatment.
- Mandatory is the simultaneous treatment of the partner, even if he has no clinical manifestations. Otherwise, it will not be possible to achieve positive dynamics.
Treatment is accompanied by a number of recommendations and rules. For example, a woman will need to stop drinking alcohol and exclude any unprotected sex (sex is only possible with a condom). Topical treatment is excluded for the duration of menstruation. A daily shower, shaving of the external genital hair, regular change of underwear, use of individual towels/bed linen are mandatory.
Both local and general therapies are used for treatment. This allows you to have a local effect on the infectious agent and at the same time eliminate the symptoms. The main drugs for treating trichomoniasis in women are 5-nitroimidazole derivatives. These are DNA-tropic drugs that have selective activity against the pathogen. Penetrating into T. vaginalis cells, the drug becomes a highly toxic metabolite that destroys nucleic acids. The advantage of such drugs is that they are highly bioavailable and do not require intravenous administration. Their effectiveness is not affected by food intake, and when administered vaginally and intrarectally they are well absorbed and have almost instantaneous action.
Also in the treatment of urogenital trichomoniasis, nitrofurans can be used. These drugs additionally have activity against Gram-positive and Gram-negative microorganisms, so they can be used in the therapy of mixed infections. The action of nitrofurans is based on the ability to destroy cellular respiration of microorganisms by inhibiting DNA synthesis. As a result of this process, nitrofuran metabolites are formed, which destroy the growth, development and division of T. vaginalis cells. The drugs are well absorbed from the gastrointestinal tract and have high bioavailability.
Treatment of the chronic form of the disease involves a comprehensive approach, including measures to increase the body’s defenses. In these cases, nonspecific immunotherapy is used.
A special approach is required when treating patients during pregnancy. Therapy for the disease is carried out at any stage, and the prognosis in the majority of cases is favorable. However, there is still no clear information on whether the therapy can prevent the development of perinatal complications. Therefore, it is best if diagnosis and treatment of the infection are carried out at the planning stage of pregnancy.
A repeat smear test for trichomoniasis will be required to monitor the results in women. In this case, as a rule, the same technique is used as at the stage of initial diagnosis. The procedure is carried out 14 days after the end of therapy. If the result of the study is negative, the patient does not need further monitoring. If the result is positive, the doctor may prescribe other medications and treatment methods. At this stage it is important to rule out reinfection, i.e. reinfection.
In general, the prognosis is favorable, since in almost all cases a complete cure is achieved. But we advise you not to forget that it is better to prevent the development of STDs than to treat their consequences. Be more attentive to your own health and don’t neglect preventive check-ups with your doctor!











I received the package a few days ago. Thank you so very much! Everything was perfect. I do appreciate your great service and will most definitely order again from you. I'm glad to say that I can recommend you with total confidence. Thanks
Yeah! The package arrived very quickly. Thanks!
Everything is fine! Thanks!